Requirements
3.1 Overview
FIGURE 1 illustrates a typical community shared care context. There are two places health record systems might be used: at the community level, that is, inter-provider, and within providers. The first kind of a record -a shared care record (longitudinal, comprehensive, patient-centred) -is classified by ISO (TS 18308) as an “EHR”, or Electronic Health Record. Some providers also have intra-provider records (episodic, institution-centred) which are usually known as EMRs (Electronic Medical Records) or EPRs (Electronic Patient Records). Others need to connect directly with the EHR. Within larger health system contexts -provinces and nations - there may also be so-called “summary health records”, or “health summaries”. The figure shows the shared care EHR as if it is located within a geographical community, but this need not be so: mobile patients such as health workers, entertainers, athletes and the military may well be represented in the same kind of system (from an IT point of view), where the contributing providers are located all over the world. Essentially, the only difference between the two is the network deployment.
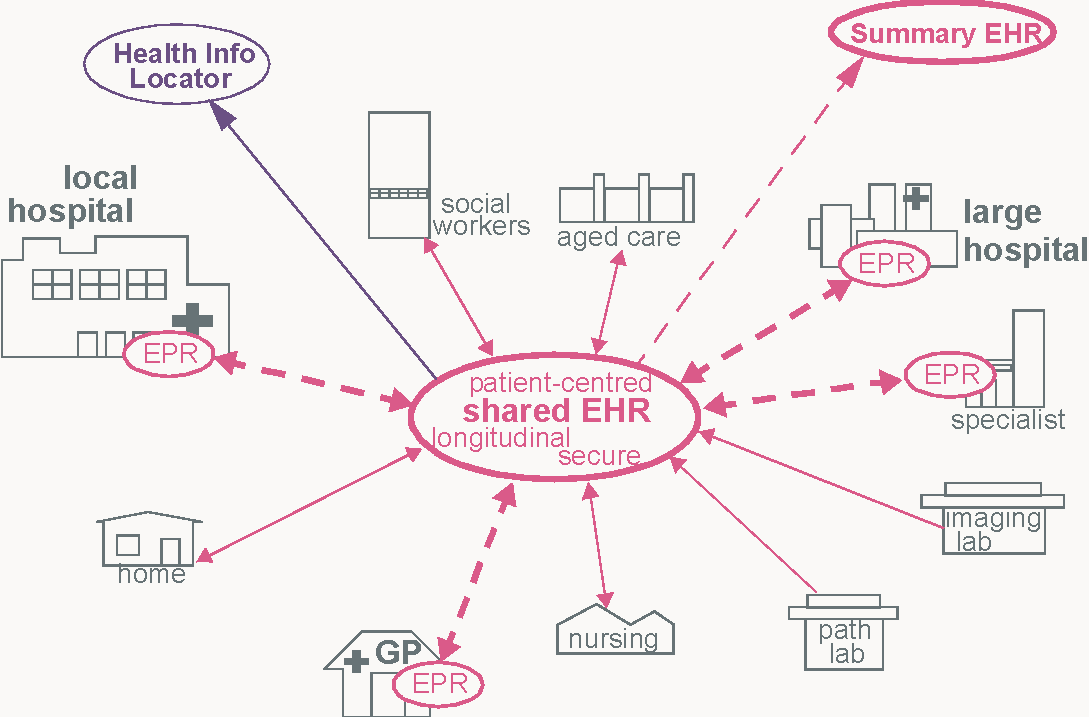
FIGURE 1 Community Shared Care Context
Health record systems built according to openEHR and related specifications could be used in any of these three locations; the health record at each level will then be in exactly the same technology and logical data format, and differ only in content, for example as follows.
- EPR/EMR: contents reflect only certain episodes, and possibly particular medical specialties, but in the greatest level of detail (outside of dedicated imaging and other monitoring systems).
- EHR: contents reflect all episodes in all providers in the community, and all medical specialties, but may be somewhat summarised, with certain intermediate details of care during certain episodes not included or greatly summarised. The EHR needed by all providers in
• Health Summary: contents probably include only core information that is needed for accident/emergency care admissions, such as basic data (blood type, age, sex), major problems, therapeutic precautions (allergies, cultural preferences) and so on.
Care events that happen while a patient is out of his or her usual context (on holiday, at a conference) will most likely initially be recorded in an EMR system not connected to the health information environment containing the principal instance of the patient’s EHR. To perform the care, the provider in question will need to be able to obtain an extract from the patient’s primary EHR; for the latter to be kept up to date, an extract will need to be sent back containing details of the foreign care event. Such interactions are mediated by a Health Information Location service (of the kind defined by the OMG HILS specification for example).
Of the three kinds of record system, the first two - the EMR and EHR - are care-oriented, and will have user software applications accessing and writing to them. Summary EHR systems will most likely have write access due to uploading of EHR Extracts, and read access.
3.2 Scenarios
The system interfaces covered by this specification include the following:
- user (client) to EHR or EMR server (real-time read/write per patient record)
- query interface to EHR or EMR (real-time or batched access to multiple records, including pseudonymisation capability)
- EMR server to EHR server (publishing with summarisation)
- EHR server to Summary server (publishing with summarisation)
- EHR to EHR Server (synchronisation or move of patient record)
- EMR or EHR to HILS (publishing)
This specification describes formal, functional interfaces between systems which correspond to these scenarios.